Impact of a Pharmacy Care Management Service on Medically Complex Medicare Advantage Members
Read the whitepaper here.
Introduction
The Medicare Advantage (MA) program has seen substantial growth in the past two decades, and much of that growth has come form medically complex health plan members who have multiple chronic conditions. This will have a major impact on utilization, costs, and quality in the MA program.
A recent 12-month study conducted by Mosaic Pharmacy Service in partnership with UPMC Health Plan focuses on health service utilization and total cost of care for medically complex members of MAPD plans operated by UPMC. Mosaic’s initiative involves the design, implementation, and evaluation of a pharmacy care management (PCM) program for MA members with multiple chronic conditions, aiming to optimize medication use and potentially avoid costly health services.
The analysis, conducted by a research team from UPMC Health Plan and RxAnte, validates that the added costs of a targeted program that includes pharmacist care management, medication reconciliation and medication in easy-to-use packaging delivered to the patient’s home lowers net costs while improving medication adherence and member satisfaction.
“We learned that an analytically targeted, coordinated and thoughtful Pharmacy Care Management approach can help Medicare Advantage members save money and improve their health outcomes,” said co-author Chronis Manolis, R. Ph., chief pharmacy officer at UPMC Health Plan. “In addition to helping individual patients, this ultimately lowers downstream health care costs and utilization.”
Design
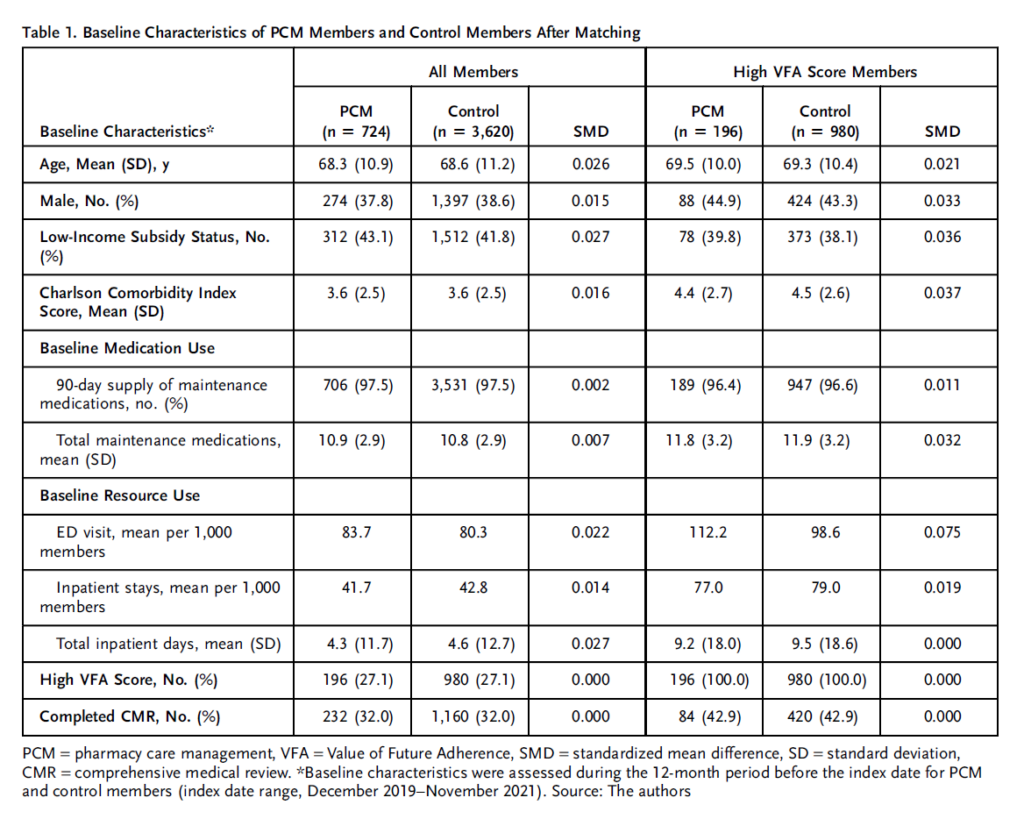
The goal of the study was to investigate the impact of an integrated PCM program for MA beneficiaries taking multiple chronic medications, including a subset with high predicted cost savings from improved medication adherence, assessed using the Value of Future Adherence (VFA) score. A total of 724 members receiving PCM services were matched to 3,620 control members who received usual pharmacy care. The average PCM participant was 68 years old and 38% were male. Participants took an average of 11 maintenance medications daily.
Intervention
The PCM program did not include members in state-sponsored pharmaceutical assistance programs or those using pharmacies with similar services. Mosaic Pharmacy Service provided the following services:
- Contacted monthly by a pharmacist or certified pharmacy technician
- Clinical pharmacy services including:
- Caregiver education, healthcare provider referrals, consultation with prescribers on medication regimen changes, referral to social support/case management programs from MAPD plan
- Specialized medication dispensing services- home delivery in 30-day cycles in a box of pre-sorted pouches with a large label of visuals and instructions for each medication affixed to the box
Results
Cost of Care
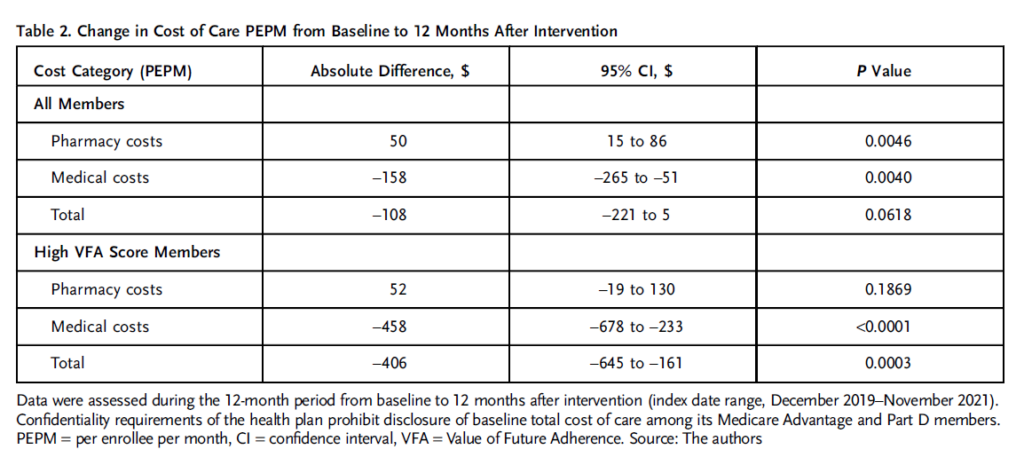
- PCM Members with High VFA Scores
- Increase in pharmacy spending ($52 PEPM)
- Offset decrease in medical spending ($458 PEPM)
- Lower total cost of care ($406 PEPM)
Health Services Use
- PCM Members with High VFA Scores
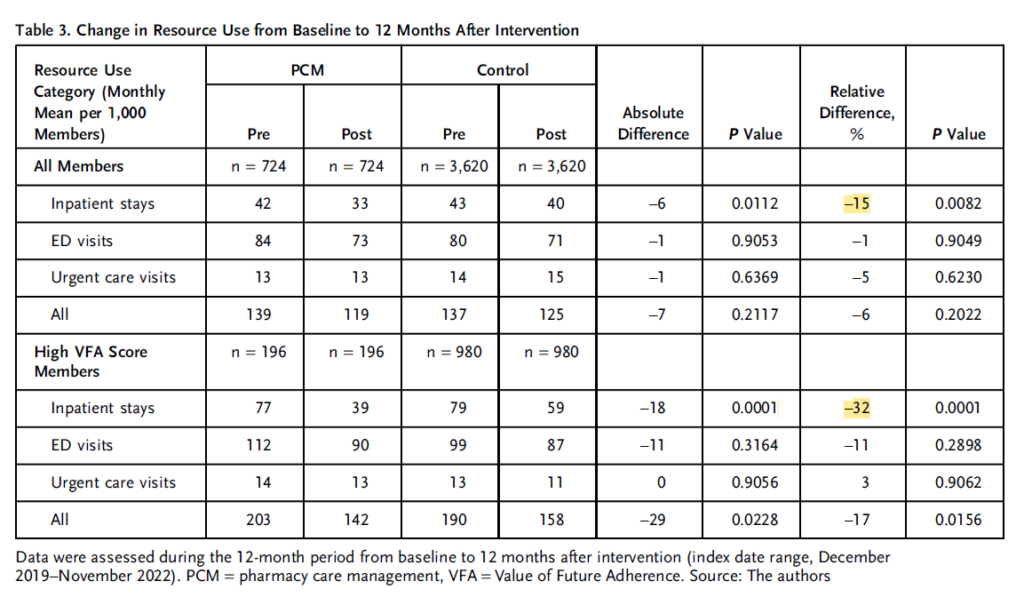
- All resource use (inpatient stays, ED visits, and urgent care visits) was 17% lower
- 32% fewer inpatient stays per 1,000 member months compared with control members
Medication Adherence with PCM
- There was a significant increase in adherence rates for oral antidiabetic therapy, renin-angiotensin system antagonists, and statins among PCM members. The improvements ranged from from 12.2% to 14.3% for those with a high Value of Future Adherence (VFA) score.
Conclusion
Read the whole case study here. Interested in learning how Mosaic can help your health plan improve medication use among your most complex Part D membership? Contact us today to learn more.